Common Disease Could Be Why Your Fingers Turn a Different Colour in Cold Winter Months

Millions of people experience an unusual reaction when they get cold. Their extremities, particularly their fingers and toes, change color. For many, this phenomenon might be alarming, especially when their fingers turn a pale white or dark red. However, this reaction is far from uncommon, and there’s actually a medical explanation for it. The condition that causes this color change is called Raynaud’s disease or Raynaud’s phenomenon, and while it may seem worrisome, it is a condition that affects millions of people—often without them even realizing they have it.
What Is Raynaud’s Disease?
Raynaud’s disease, sometimes called Raynaud’s phenomenon, is a condition that primarily affects the circulation in your extremities—your fingers and toes. This disease causes the blood vessels in these areas to constrict or narrow, restricting blood flow, especially when exposed to cold temperatures or stress.
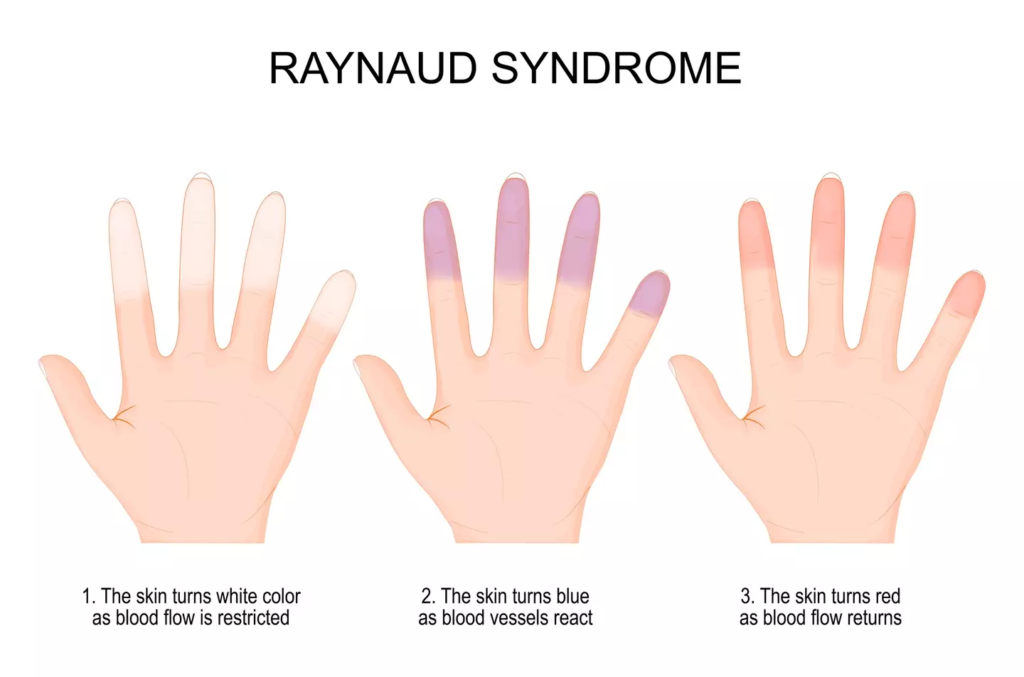
When this happens, the extremities can change color, often turning white, blue, or red depending on the stage of the attack. The color changes can be startling at first, leading many people to wonder if there’s something seriously wrong with their bodies. However, for the majority of those who experience it, Raynaud’s is not a serious health issue, though it can be uncomfortable.
Raynaud’s is a vascular condition that is most often triggered by cold weather or emotional stress. However, in some cases, it may occur due to other underlying health conditions such as autoimmune diseases, or even as a side effect of certain medications. The good news is that Raynaud’s disease is relatively common, and there are ways to manage it.

To dive deeper into understanding the condition and how it affects your body, check out the Raynaud’s Association for more information.
What Happens When You Have Raynaud’s Disease?
When a person with Raynaud’s disease is exposed to cold weather, their blood vessels constrict in response, cutting off circulation to the fingers, toes, and sometimes other extremities like the ears, nose, or lips. This reduction in blood flow causes the affected areas to turn white, and in some cases, blue, as the oxygen in the blood is depleted. Once the vessels dilate again and blood flow is restored, the areas will often turn red due to the rush of oxygenated blood.
The key symptoms of Raynaud’s disease include:
- Color changes: Fingers, toes, or other extremities may turn white, blue, or red.
- Coldness: The affected areas feel extremely cold to the touch.
- Numbness or tingling: As blood flow decreases, you might feel a tingling or “pins and needles” sensation.
- Pain: The affected areas may also experience pain due to the restricted blood flow.
These symptoms can appear suddenly, and in some cases, they can last from a few minutes to several hours.
If you’re experiencing any of these symptoms frequently or they become severe, it’s important to talk to a healthcare provider. Understanding the root cause of the problem can help you find the most effective way to manage the condition.
The Impact of Cold Weather and Stress on Raynaud’s Disease
Cold weather is one of the most common triggers of Raynaud’s phenomenon, and it can make the condition more noticeable. During winter months or on especially cold days, people with Raynaud’s may find that their fingers and toes quickly turn white or blue, and the discomfort can be intense. This is because, when exposed to extreme cold, the body prioritizes warming the core over the extremities, leading to restricted blood flow to fingers and toes.
In addition to cold, emotional stress is another common trigger. Stress can cause the body to release stress hormones that lead to vasoconstriction, which is the narrowing of blood vessels, leading to similar color changes. For people who experience both cold-induced and stress-induced episodes, managing stress and staying warm are key factors in controlling the condition.

You can learn more about Raynaud’s triggers and how to avoid them by visiting the American Heart Association’s site on Raynaud’s.
Raynaud’s Symptoms and Other Affected Areas
In addition to the color changes and coldness of your fingers and toes, Raynaud’s disease can also cause other sensations in the affected areas, such as numbness and pins and needles. These symptoms can be quite discomforting and are caused by the lack of blood flow to the tissues in these regions. In some cases, the skin may even appear shiny, or the nails may appear deformed due to prolonged exposure to the condition.
Although Raynaud’s disease typically affects the hands and feet, it can also impact other areas of the body, including:
- Ears
- Nose
- Lips
- Nipples
In rare cases, when Raynaud’s is severe or chronic, it can lead to more serious complications, such as ulcers or even tissue damage. However, these more severe complications are uncommon, and most people can manage their symptoms through lifestyle changes, appropriate clothing, and medications if needed.
If you are experiencing Raynaud’s symptoms in multiple areas of your body, it is a good idea to schedule a check-up with your doctor to discuss potential treatments and understand whether there may be an underlying cause.
Should You See a Doctor About Raynaud’s Disease?
If you experience Raynaud’s symptoms regularly or if they become more severe, it’s important to consult with a healthcare professional. While Raynaud’s is typically not dangerous, it can lead to more serious complications if left unchecked, especially if it’s secondary to an underlying condition like lupus or scleroderma. A doctor can help determine whether the condition is primary (meaning it occurs on its own) or secondary (meaning it is related to another disease) and offer recommendations for treatment.
Dr. Melisa Lai Becker, an expert in vascular diseases, advises those experiencing painful or persistent symptoms to visit a doctor. Raynaud’s can sometimes be caused or worsened by certain medications, so it’s essential to discuss any medications you’re currently taking with your healthcare provider.
If you’re unsure whether your symptoms are related to Raynaud’s disease, you can read more about diagnosis and treatment options at the Mayo Clinic’s Raynaud’s Disease Page.
Risk Factors: Who Is Most Affected by Raynaud’s?
Raynaud’s disease is overwhelmingly more common in women, with most people experiencing their first episode during adolescence or early adulthood. As many as 20 percent of adults worldwide may be affected by some form of Raynaud’s. This condition is also more common in individuals who live in colder climates, as extreme temperatures can trigger the symptoms more often.
While Raynaud’s affects people of all ages, certain factors may increase the likelihood of developing the disease, including:
- Genetics: Family history of Raynaud’s or other autoimmune conditions can increase the risk.
- Climate: Those living in colder regions are more likely to develop the disease.
- Health conditions: Certain diseases like scleroderma, lupus, and rheumatoid arthritis can increase the risk of developing secondary Raynaud’s.
If you have a family history of Raynaud’s or autoimmune diseases, it may be helpful to monitor your symptoms and talk to a healthcare provider about preventive care.
For more on the risk factors and management tips, check out the detailed guide on WebMD’s Raynaud’s Disease Overview.
Conclusion: Managing Raynaud’s Disease
While Raynaud’s disease can be uncomfortable, it’s typically not a cause for alarm. Most people with Raynaud’s can manage their symptoms with simple changes to their lifestyle, such as dressing warmly, managing stress, and avoiding prolonged exposure to cold. In some cases, medications may be required to improve blood flow or to address underlying health conditions.
If you notice that your fingers or toes frequently change color and become numb in cold weather, it’s worth consulting a healthcare provider to rule out other potential causes. Understanding your condition and learning how to prevent attacks can greatly improve your quality of life, especially in the winter months.
For further guidance on managing Raynaud’s disease, check out the Raynaud’s Association or talk to your doctor for personalized advice.
Featured Image Credit: Getty Stock Images